Scientists have succeeded in turning stem cells into insulin-producing cells
San Francisco researchers have succeeded in transforming human stem cells into mature insulin-producing cells. The achievement opens the door to developing new, effective therapies against type 1 diabetes.
Research conducted at the University of California San Francisco (UCSF) may helpoc millions of waspsob suffering from type 1 diabetes. For the first time, it has been possible to transform cellsostem cells into comoinsulin-producing cells, which may represent a breakthrough in efforts to develop an effective drug for the disease.
Replacement of lost comorek new, whichore produce insulin in the patientow with type 1 diabetes has long been a medical dream, but until now scientists have not been able to come up with a good way to produce comorki in a laboratory vessel, whichore function exactly as in healthy adults. Now the California researchers have succeeded in doing so.
The results of the study were published in „Nature Cell Biology”.
Type 1 diabetes is an autoimmune disorder. The body itself destroys insulin-producing comobeta cells of the pancreas, and without insulin and its ability to regulate blood glucose levels, high concentrations of sugar can cause serious damage to the organ’sow, and even death. This disease can be managed with regular injections ofoin insulin, but despite this, affected individuals still often experience serious health consequences such as kidney failure and heart disease.
– We can now generate comorks that produce insulin, whichore look and act similarly to comorki beta pancreas, whichore we all have in our bodies. This is an important step toward our goal of creating comorek, ktore can be transplanted into patients with diabetes – said Dr. Matthias Hebrok of UCSF, one of the authors of theoin publications.
Patients suffering from life-threatening complications may qualify for a pancreas transplant from a deceased donor, but these are rare cases and waiting times are very long. Of the approximately 1.5 million people living with type 1 diabetes in the U.S., only about 1,000 get pancreas transplants. The procedure is roalso risky: recipients must take immunosuppressive drugs for life, and many of the transplantsow ends in failure for one reason or another. The subject of the study is transplantation only „pancreatic islets" – clusters of comorecords containing healthy cellsork beta cells, but several major problems have been encountered in this fieldow and work, although advancing, has not yet become a widely used solution.
Scientists searching for a cure for type 1 diabetes for years prob they transformed the comostem cells in the comobeta cells. They have pinned great hopes on this. The use of comostem cells to culture healthyobeta sharks, whichore then can be transplanted into patients, would be an excellent solution. The problem was the transformation of the comostem cells into fully mature comorki beta.
– Komorks produced by us and other research teams are stuck at an immature stage, in which theorym were unable to respond appropriately to blood glucose levels. This was a major limitation in the field – admitted Hebrok.
California scientists realized that the key to developing lab-grown comobeta re to become fully mature is an overlooked physical process, in which theorym comorks separate from the rest of the pancreas and form so-called islets of Langerhans.
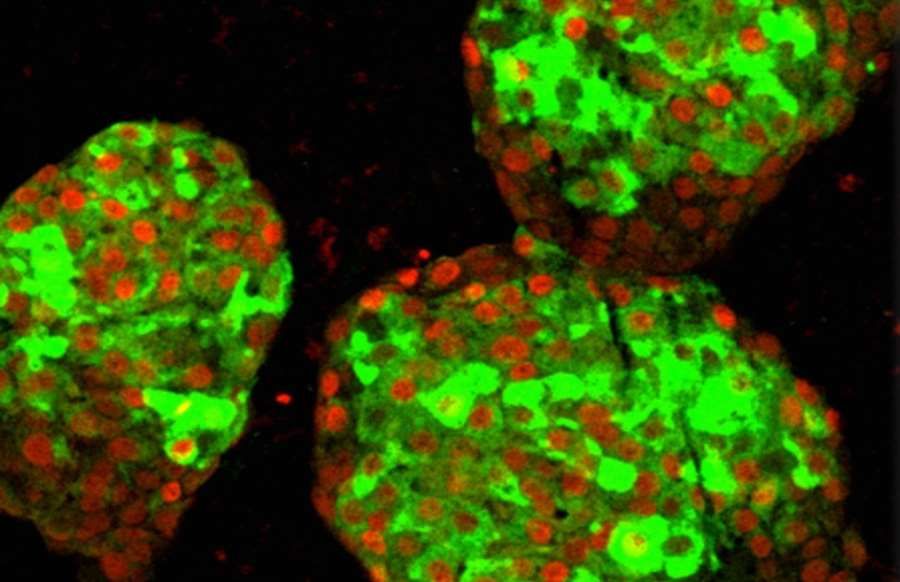
When the researchers repeatedoied this process in laboratory vessels by artificially separating partially zroof comorec pancreatic cells and transforming them into clusters resembling islets of Langerhans, developing aoj comorec suddenly jumped naprzod. Not only do the cellsobeta cells began to respond to blood sugar levels more like mature cellsoinsulin-producing cells, but the entire surroundings of the cluster – including poorly understood comoalpha and delta – roalso seemed to develop in a wayob, ktory has never been seen in laboratory culture.
The cells created in this wayork beta scientists have tested on mice. They transplanted the lab-grown clusters into rodents and observed that they began producing insulin within just a few days.
– Current therapies, such as insulin injections, only treat the symptoms of type 1 diabetes, said the study leader Dr. Gopiki Nair. – Our work points to some exciting drog, due to whichorym it will eventually be possible to find a cure for the disease – added.
– Finally, we are able to pogo forward on many roThe body itself destroys insulin-producing cells on various fronts, whichore previously unavailable to us. The possibilities seem endless – explained Hebrok.
Of course, as with any mouse study, there is still a lot of work to be done before the California researchers’ achievement becomes a helpful therapy for humans. However, the American scientists’ achievement is a huge step forwardod in this direction.
Sourceocontributed by University of California San Francisco, fot. Hebrok Lab / UCSF. Pictured are clusters of pancreatic comobeta records derived from human pluripotent cellsostem cells in a laboratory dish. Komoinsulin-producing rks are marked in green. Red indicates the presence of PDX1, a key protein involved in insulin production.